- Thyroid
- Hashimoto Thyroiditis and Mortality in Patients with Differentiated Thyroid Cancer: The National Epidemiologic Survey of Thyroid Cancer in Korea and Meta-Analysis
-
Injung Yang, Jae Myung Yu, Hye Soo Chung, Yoon Jung Kim, Yong Kyun Roh, Min Kyu Choi, Sung-ho Park, Young Joo Park, Shinje Moon
-
Endocrinol Metab. 2024;39(1):140-151. Published online January 3, 2024
-
DOI: https://doi.org/10.3803/EnM.2023.1748
-
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader  ePub ePub
- Background
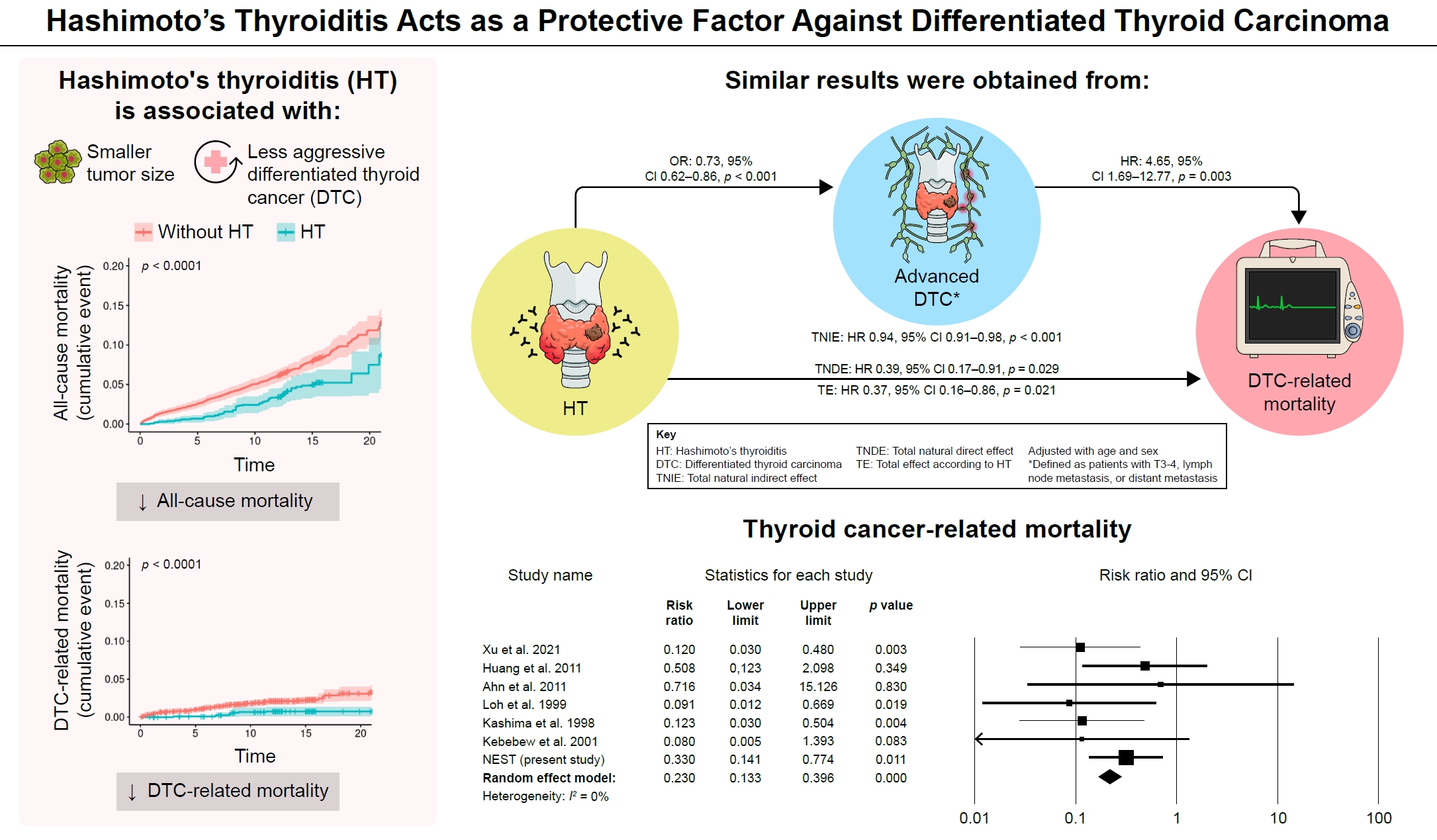
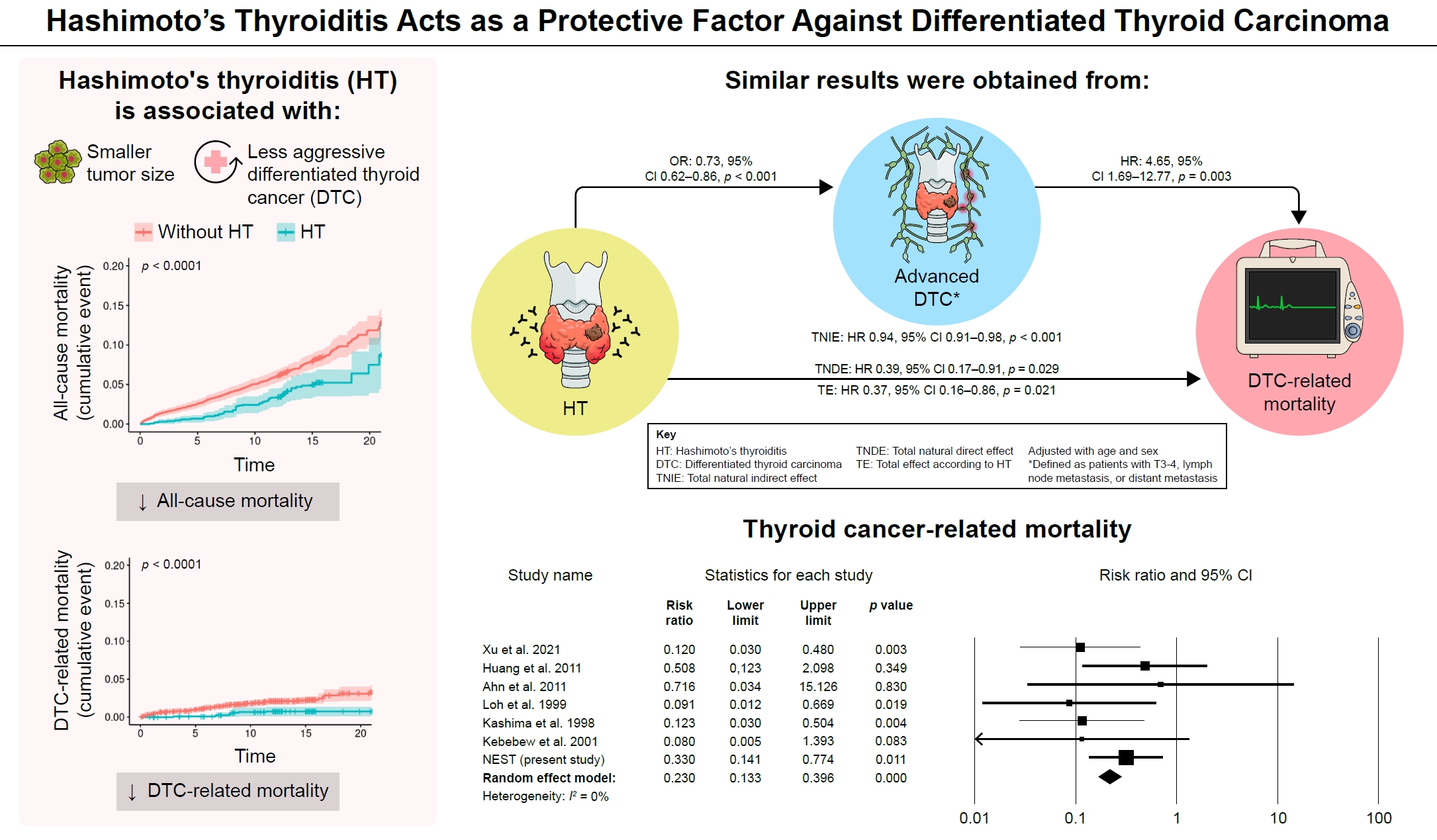
Many studies have shown that Hashimoto’s thyroiditis (HT) acts as a protective factor in differentiated thyroid cancer (DTC), but little is known about its effects on mortality. Therefore, this study was performed to reveal the prognosis of HT on mortality in patients with DTC.
Methods
This study included two types of research results: retrospective cohort study using the National Epidemiologic Survey of Thyroid cancer (NEST) in Korea and meta-analysis study with the NEST data and eight selected studies.
Results
Of the 4,398 patients with DTC in NEST, 341 patients (7.8%) died during the median follow-up period of 15 years (interquartile range, 12.3 to 15.6). Of these, 91 deaths (2.1%) were related to DTC. HT was associated with a smaller tumor size and less aggressive DTC. In Cox regression analysis after adjusting for age and sex, patients with HT showed a significantly lower risk of all-cause death (hazard ratio [HR], 0.71; 95% confidence interval [CI], 0.52 to 0.96) and DTC-related death (HR, 0.33; 95% CI, 0.14 to 0.77). The analysis with inverse probability of treatment weight data adjusted for age, sex, and year of thyroid cancer registration showed similar association. The meta-analysis showed that patients with HT showed a lower risk of all-cause mortality (risk ratio [RR], 0.24; 95% CI, 0.13 to 0.47) and thyroid cancer-related mortality (RR, 0.23; 95% CI, 0.13 to 0.40) in comparison with patients without HT.
Conclusion
This study showed that DTC co-presenting with HT is associated with a low risk of advanced DTC and presents a low risk for all-cause and DTC-related death.
- Clinical Study
Big Data Articles (National Health Insurance Service Database)
- Variabilities in Weight and Waist Circumference and Risk of Myocardial Infarction, Stroke, and Mortality: A Nationwide Cohort Study
-
Da Hye Kim, Ga Eun Nam, Kyungdo Han, Yang-Hyun Kim, Kye-Yeung Park, Hwan-Sik Hwang, Byoungduck Han, Sung Jung Cho, Seung Jin Jung, Yeo-Joon Yoon, Yong Kyun Roh, Kyung Hwan Cho, Yong Gyu Park
-
Endocrinol Metab. 2020;35(4):933-942. Published online December 23, 2020
-
DOI: https://doi.org/10.3803/EnM.2020.871
-
-
5,566
View
-
110
Download
-
15
Web of Science
-
16
Crossref
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader  ePub ePub
- Background
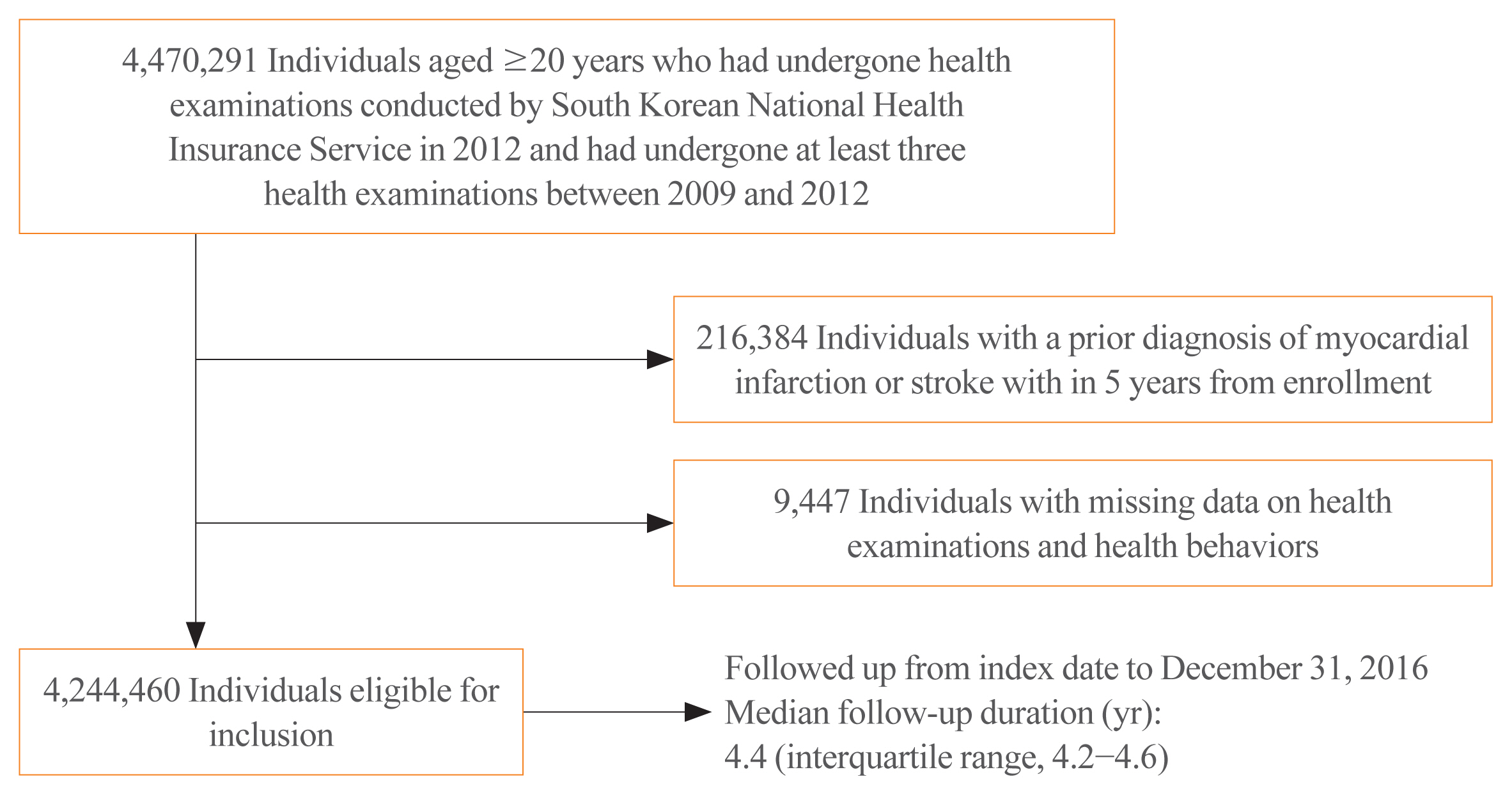
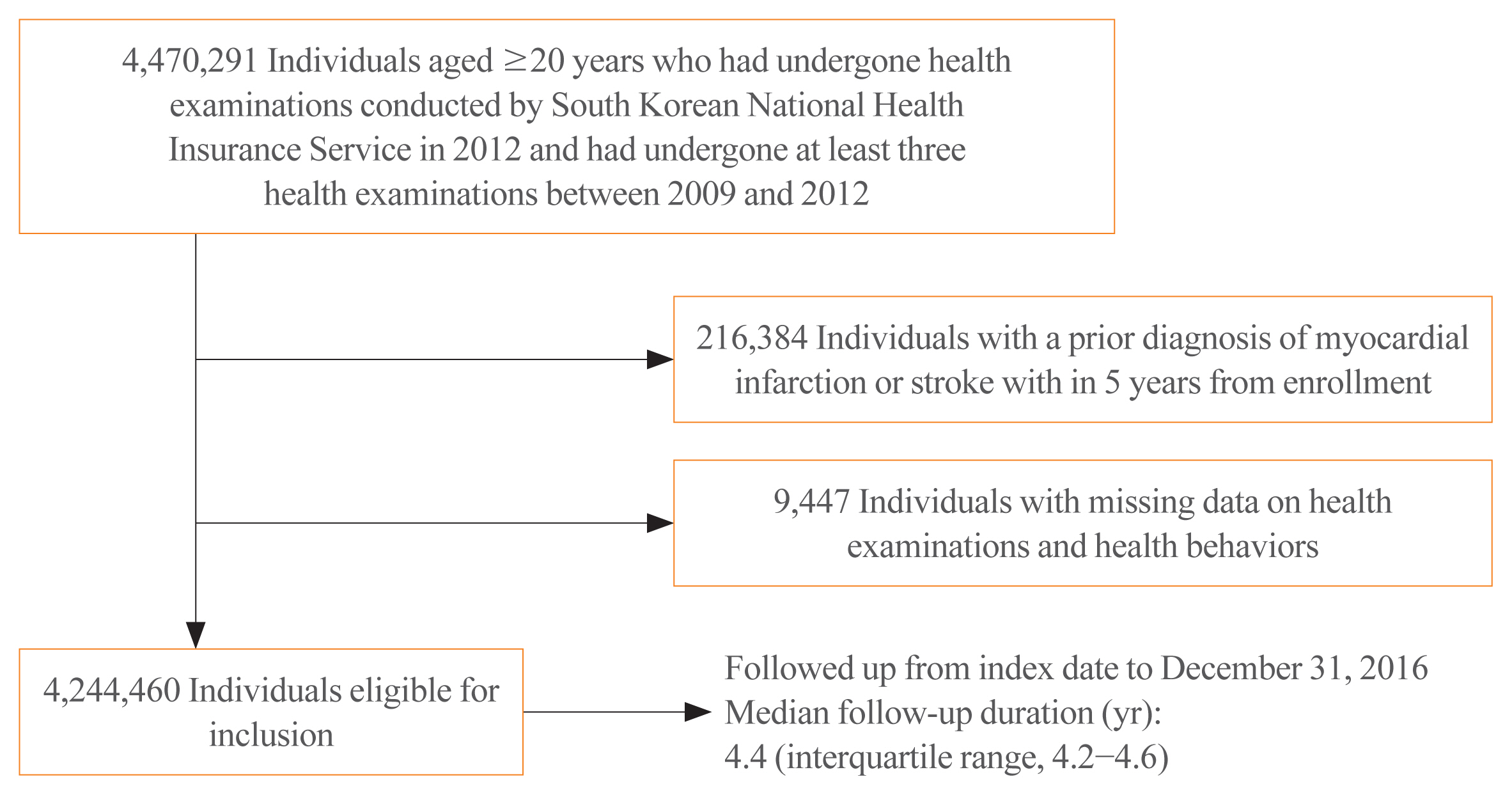
Evidence regarding the association between variabilities in obesity measures and health outcomes is limited. We aimed to examine the association between variabilities in obesity measures and cardiovascular outcomes and all-cause mortality.
Methods
We identified 4,244,460 individuals who underwent health examination conducted by the Korean National Health Insurance Service during 2012, with ≥3 anthropometric measurements between 2009 and 2012. Variabilities in body weight (BW) and waist circumference (WC) were assessed using four indices including variability independent of the mean (VIM). We performed multivariable Cox proportional hazards regression analyses.
Results
During follow-up of 4.4 years, 16,095, 18,957, and 30,200 cases of myocardial infarction (MI), stroke, and all-cause mortality were recorded. Compared to individuals with the lowest quartiles, incrementally higher risks of study outcomes and those of stroke and all-cause mortality were observed among individuals in higher quartiles of VIM for BW and VIM for WC, respectively. The multivariable adjusted hazard ratios and 95% confidence intervals comparing the highest versus lowest quartile groups of VIM for BW were 1.17 (1.12 to 1.22) for MI, 1.20 (1.16 to 1.25) for stroke, and 1.66 (1.60 to 1.71) for all-cause mortality; 1.07 (1.03 to 1.12) for stroke and 1.29 (1.25 to 1.33) for all-cause mortality regarding VIM for WC. These associations were similar with respect to the other indices for variability.
Conclusion
This study revealed positive associations between variabilities in BW and WC and cardiovascular outcomes and allcause mortality. Our findings suggest that variabilities in obesity measures are associated with adverse health outcomes in the general population.
-
Citations
Citations to this article as recorded by  - Gender differences in midlife to later-life cumulative burden and variability of obesity measures and risk of all-cause and cause-specific mortality
Karim Kohansal, Siamak Afaghi, Davood Khalili, Danial Molavizadeh, Farzad Hadaegh
International Journal of Obesity.2024; 48(4): 495. CrossRef - Association of body mass index and blood pressure variability with 10-year mortality and renal disease progression in type 2 diabetes
Stephen Fava, Sascha Reiff
Acta Diabetologica.2024;[Epub] CrossRef - Weight variability and cardiovascular outcomes: a systematic review and meta-analysis
Robert J. Massey, Moneeza K. Siddiqui, Ewan R. Pearson, Adem Y. Dawed
Cardiovascular Diabetology.2023;[Epub] CrossRef - Family history, waist circumference and risk of ischemic stroke: A prospective cohort study among Chinese adults
Lei Liu, Xiaojia Xue, Hua Zhang, Xiaocao Tian, Yunhui Chen, Yu Guo, Pei Pei, Shaojie Wang, Haiping Duan, Ruqin Gao, Zengchang Pang, Zhengming Chen, Liming Li
Nutrition, Metabolism and Cardiovascular Diseases.2023; 33(4): 758. CrossRef - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinology and Metabolism.2023; 38(1): 10. CrossRef - Weight variability and diabetes complications
Francesco Prattichizzo, Chiara Frigé, Rosalba La Grotta, Antonio Ceriello
Diabetes Research and Clinical Practice.2023; 199: 110646. CrossRef - Research on obesity using the National Health Information Database: recent trends
Eun-Jung Rhee
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 35. CrossRef - Weight cycling and risk of clinical adverse events in patients with heart failure with preserved ejection fraction: a post-hoc analysis of TOPCAT
Yi Tan, Hang Guo, Ning Zhang, Keyang Zheng, Guifang Liu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Weight variability, physical functioning and incident disability in older adults
Katie J. McMenamin, Tamara B. Harris, Joshua F. Baker
Journal of Cachexia, Sarcopenia and Muscle.2023; 14(4): 1648. CrossRef - Association between Variability of Metabolic Risk Factors and Cardiometabolic Outcomes
Min Jeong Park, Kyung Mook Choi
Diabetes & Metabolism Journal.2022; 46(1): 49. CrossRef - Effects of exercise initiation and smoking cessation after new-onset type 2 diabetes mellitus on risk of mortality and cardiovascular outcomes
Mee Kyoung Kim, Kyungdo Han, Bongsung Kim, Jinyoung Kim, Hyuk-Sang Kwon
Scientific Reports.2022;[Epub] CrossRef - Lipid cutoffs for increased cardiovascular disease risk in non-diabetic young people
Mee Kyoung Kim, Kyungdo Han, Hun-Sung Kim, Kun-Ho Yoon, Seung-Hwan Lee
European Journal of Preventive Cardiology.2022; 29(14): 1866. CrossRef - Body Mass Index Is Independently Associated with the Presence of Ischemia in Myocardial Perfusion Imaging
Chrissa Sioka, Paraskevi Zotou, Michail I. Papafaklis, Aris Bechlioulis, Konstantinos Sakellariou, Aidonis Rammos, Evangelia Gkika, Lampros Lakkas, Sotiria Alexiou, Pavlos Kekiopoulos, Katerina K. Naka, Christos Katsouras
Medicina.2022; 58(8): 987. CrossRef - Waist Circumference and Body Mass Index Variability and Incident Diabetic Microvascular Complications: A Post Hoc Analysis of ACCORD Trial
Daniel Nyarko Hukportie, Fu-Rong Li, Rui Zhou, Jia-Zhen Zheng, Xiao-Xiang Wu, Xian-Bo Wu
Diabetes & Metabolism Journal.2022; 46(5): 767. CrossRef - Nonalcoholic fatty liver disease and the risk of insulin-requiring gestational diabetes
Sang Youn You, Kyungdo Han, Seung-Hawn Lee, Mee Kyoung Kim
Diabetology & Metabolic Syndrome.2021;[Epub] CrossRef - Increased Risk of Nonalcoholic Fatty Liver Disease in Individuals with High Weight Variability
Inha Jung, Dae-Jeong Koo, Mi Yeon Lee, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
Endocrinology and Metabolism.2021; 36(4): 845. CrossRef
|